Digital Twins for Opioid Use Disorder: Replacing Trial and Error With Predictive Care


Opioid use disorder remains one of healthcare’s most complex clinical and operational challenges, driven by wide patient variability and limited ability to predict treatment response. In a HealthAI Collective lightning talk, Albert Burgess-Hull explains how digital twins can help care teams move beyond trial and error by modeling individual patient trajectories, improving treatment selection, and enabling more precise, data-driven decisions at scale.
Medications for opioid use disorder such as buprenorphine and methadone are the gold standard of care. When taken consistently, they reduce cravings, opioid use, overdose risk, and mortality but the challenge is variability.
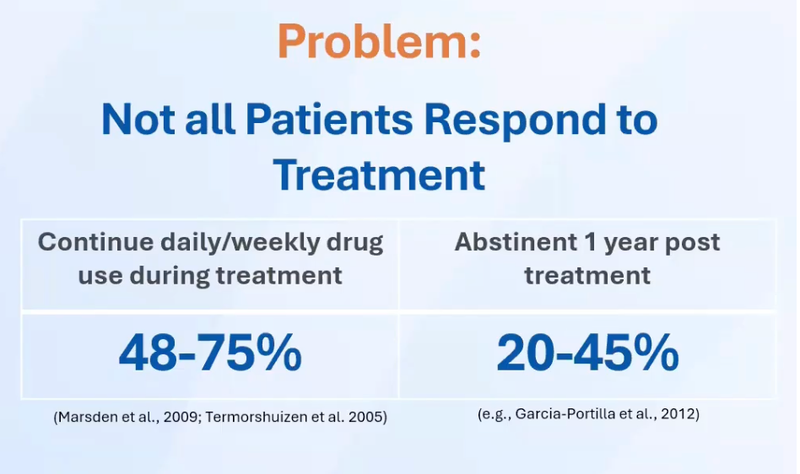
As described in the talk, a significant portion of patients continue using opioids during and after treatment. Care teams lack predictive tools to identify who will respond and who will not. The result is a wait and see approach where weeks or months can pass before it becomes clear that a treatment plan is failing but in opioid use disorder, those delays can be fatal.
From an executive perspective, this model also wastes scarce clinical resources, over treats some patients, under treats others, and introduces unnecessary operational friction.
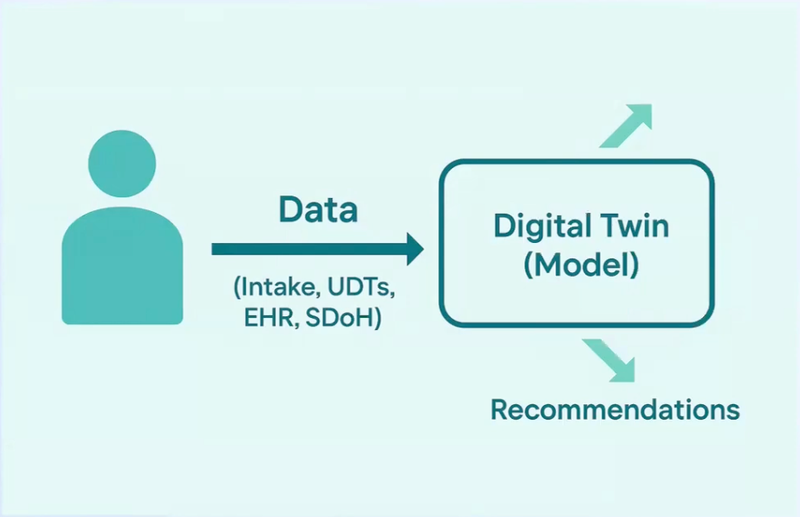
A digital twin is a continuously updated computational representation of a specific entity. In healthcare, that entity can be a patient, a clinic, or a treatment pathway.
What makes digital twins powerful is their ability to simulate counterfactuals. Teams can test what-if scenarios and forecast outcomes before acting in the real world.
This capability shifts decision making from reactive to predictive, which is essential in high-risk clinical domains.
Dr. Albert Burgess-Hull, Founder and CEO of DeepCare Labs, introduced the concept of a treatment twin for opioid use disorder.
The treatment twin is a real time digital prognostic framework that ingests the intake data and urine toxicology results to predict an individual patient’s response to treatment. Predictions are updated at each appointment, creating a dynamic view of patient risk over time.
Instead of treating all patients the same, the system:
This approach replaces subjective judgment with data driven foresight.
Traditional clinical assessments rely heavily on cross sectional data. The treatment twin focuses on trajectories.
Using longitudinal urine toxicology data from thousands of patients, the framework identifies distinct response patterns over time. Patients cluster into subgroups such as consistent responders, gradual responders, gradual return to use, and consistent non-responders.
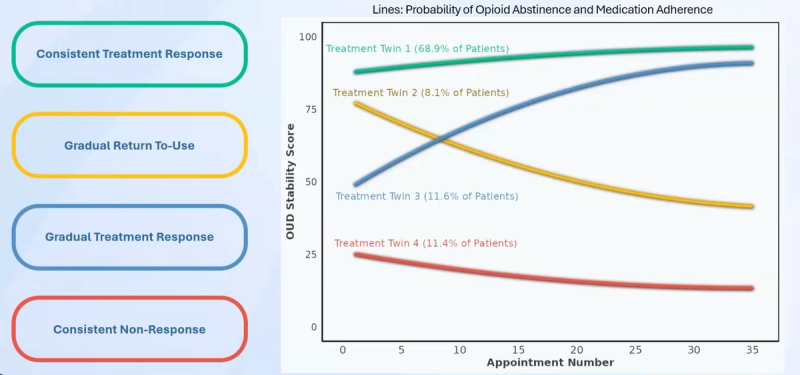
As additional data is collected, prediction accuracy improves rapidly. This highlights a critical executive insight.
Dynamic, adaptive systems compound value over time. Static decision tools do not.
For healthcare executives, the implications extend beyond addiction medicine.
As Burgess-Hull noted:
Digital twins directly address this gap.
Precision medicine is often framed as a clinical benefit. This talk makes clear it is also an operational one.
By predicting risk early:
The result is better outcomes with the same or fewer resources. For enterprise healthcare organizations, this is the definition of sustainable ROI.
Dr. Albert Burgess-Hull is an addiction scientist and machine learning researcher, Founder and CEO of DeepCare Labs, and Scientific Director of SUDx. His work focuses on digital health systems and digital twins to improve medical decision making, operational efficiency, and substance use disorder treatment. He received his PhD from the University of Wisconsin - Madison and completed postdoctoral training at the National Institutes of Health.
Using Digital Twins for the treatment of Opioid Use Disorder